Exploring Kidney Health: Causes, Conditions, and Innovative Approaches
Hey there, incredible readers interested in kidney health and the cutting edge of medical science! Our kidneys are truly amazing organs, working tirelessly to filter waste, balance fluids, and keep our bodies running smoothly. But sometimes, these vital organs can face challenges, leading to complex conditions that require specialized attention and advanced treatments. Today, we’re going to shed some light on specific kidney conditions and the exciting progress being made in managing them.
At NephCure Inc., we’re driven by a singular, powerful mission: to accelerate research for rare kidney diseases and provide hope for patients worldwide. We understand the profound impact these conditions have on individuals and families, and we are relentlessly pursuing breakthroughs to improve diagnosis, treatment, and quality of life. Our commitment extends to fostering a global community of patients, researchers, and clinicians working together. Let’s explore some key areas in kidney disease, including causes and innovative treatment approaches, and how NephCure Inc. is at the forefront of this vital work!
Getting to the Root: Unpacking Focal Segmental Glomerulosclerosis Causes
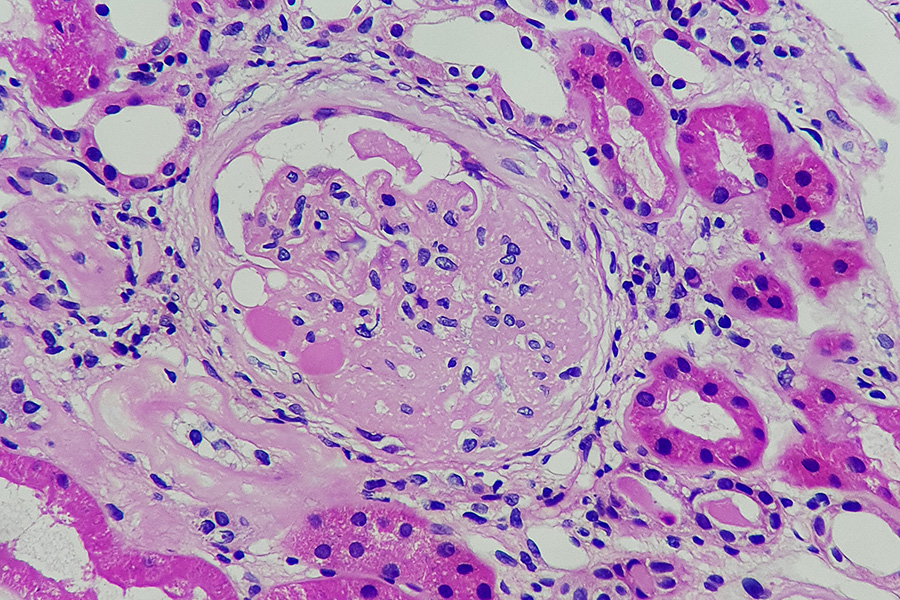
Imagine your kidneys as incredibly sophisticated filters. Within them are tiny filtering units called glomeruli. In a condition called Focal Segmental Glomerulosclerosis, or FSGS, these filters become scarred. “Focal” means only some of the glomeruli are affected, and “segmental” means only parts of those affected glomeruli are scarred. This scarring damages the filters, leading to protein leaking into the urine, which is a hallmark symptom. Identifying the Focal Segmental Glomerulosclerosis causes is crucial because it often dictates the best course of treatment.
So, what are the various Focal Segmental Glomerulosclerosis causes that researchers and clinicians identify?
- Primary (Idiopathic) FSGS: This is when there’s no identifiable cause, meaning the disease isn’t linked to another condition. It’s often thought to be caused by a circulating factor in the blood that damages the kidney’s filtering units. This form can be particularly challenging to treat.
- Genetic (Familial) FSGS: In some cases, FSGS runs in families and is caused by mutations in specific genes that are essential for the proper structure and function of the glomeruli. Over 50 different genes have been implicated, and genetic testing can help identify these predispositions.
- Examples of genes: NPHS1, NPHS2, WT1, TRPC6, INF2, ACTN4, etc.
- Implications: Genetic forms may present early in life and can sometimes respond differently to standard treatments.
- Secondary FSGS: This form develops as a consequence of another condition or factor that causes stress or damage to the glomeruli. The underlying cause needs to be addressed for effective management.
- Adapting/Compensatory FSGS: This occurs when the kidneys are under increased workload, often due to:
- Reduced Kidney Mass: For example, in individuals with only one kidney or after kidney donation.
- Obesity: Excessive weight puts a strain on kidney function over time.
- Sleep Apnea: Can lead to kidney stress.
- Hypertension (High Blood Pressure): Uncontrolled high blood pressure directly damages kidney filters.
- Drug-Induced FSGS: Certain medications can cause FSGS, including:
- Interferons: Used to treat viral infections or certain cancers.
- Pamidronate: Used to treat bone conditions.
- Anabolic Steroids: Often misused.
- Infection-Related FSGS: Some infections can trigger FSGS, such as:
- HIV-Associated Nephropathy (HIVAN): A direct kidney complication of HIV.
- Parvovirus B19: A common viral infection.
- COVID-19: Emerging evidence suggests a link between SARS-CoV-2 infection and kidney injury, including FSGS.
- Other Conditions: FSGS can also be associated with autoimmune diseases (like lupus), chronic kidney disease of other origins, or even some cancers.
- Adapting/Compensatory FSGS: This occurs when the kidneys are under increased workload, often due to:
- Collapsing FSGS: A severe variant of FSGS characterized by the collapse of the glomerular capillaries. This often has a more aggressive course and can be linked to viral infections (like HIV or Parvovirus B19) or certain medications.
Understanding the specific Focal Segmental Glomerulosclerosis causes is a cornerstone of precision medicine in nephrology. At NephCure Inc., we support groundbreaking research aimed at uncovering new causes, identifying genetic links, and developing targeted therapies based on these underlying factors.
Targeted Approaches: The Promise of C1q Treatment
The immune system is incredibly complex, designed to protect our bodies from invaders. However, sometimes it can overreact or malfunction, leading to damage to our own tissues, including the kidneys. The complement system is a part of our immune system, and a specific component called C1q plays a critical role in initiating certain immune responses. In some kidney diseases, C1q can become a target for treatment because its abnormal activity or deposition contributes to kidney damage. The concept of C1q treatment involves strategies aimed at modulating or removing C1q to reduce inflammation and preserve kidney function.
So, what does the concept of C1q treatment entail, and why is it a promising avenue for certain kidney conditions?
- Understanding C1q’s Role: C1q is the first component of the classical pathway of the complement system. When it binds to certain targets (like antibodies attached to foreign invaders, or sometimes even to damaged self-tissue), it kicks off a cascade of events that leads to inflammation and cell destruction.
- C1q Nephropathy: There’s a specific kidney disease called C1q nephropathy where C1q (and other complement proteins) are abnormally deposited in the glomeruli. This deposition contributes to kidney inflammation and damage, often leading to symptoms similar to FSGS or lupus nephritis.
- Therapeutic Strategies for C1q-Related Conditions: The goal of C1q treatment is to interfere with this harmful process. Approaches can include:
- Immunosuppression: Medications that broadly suppress the immune system, reducing the production of antibodies that might activate C1q or dampening the inflammatory response.
- Targeting Complement Components: Developing drugs that specifically block C1q or other proteins further down the complement cascade, preventing the harmful inflammatory reactions while ideally preserving other beneficial immune functions. These are often cutting-edge biological therapies.
- Plasmapheresis: A procedure that filters the blood to remove harmful antibodies or immune factors, including potentially C1q, from the circulation. This can be used in acute, severe cases.
- Research into Novel Therapies: Scientists are actively researching new molecules that can precisely modulate C1q activity or interfere with its pathological effects in the kidney.
NephCure Inc. is actively involved in funding research and advocating for the development of targeted therapies like C1q treatment that can specifically address the underlying immune dysfunctions in rare kidney diseases, moving towards more personalized and effective interventions.
Hope for the Youngest Patients: Congenital Nephrotic Syndrome Treatment
When kidney disease affects infants and very young children, it presents unique challenges. Congenital nephrotic syndrome (CNS) is a rare and severe form of nephrotic syndrome that appears within the first three months of life. It’s often caused by genetic mutations that lead to severe dysfunction of the kidney’s filters, resulting in massive protein loss in the urine, swelling, and other complications. Managing this condition requires highly specialized and often complex interventions. Therefore, advancements in Congenital Nephrotic Syndrome treatment are critical for these vulnerable patients.
So, what are the key components and current approaches in Congenital Nephrotic Syndrome treatment?
- Diagnosis and Genetic Testing: Early and accurate diagnosis is vital. Genetic testing is crucial to identify the specific gene mutation responsible (e.g., NPHS1 for Finnish type CNS, NPHS2, WT1), as this can influence prognosis and treatment options.
- Aggressive Symptomatic Management: The initial focus is on managing the severe symptoms caused by massive protein loss:
- Albumin Infusions: To replace the protein lost in urine, helping to reduce severe swelling (edema).
- Diuretics: Medications to help the body excrete excess fluid and reduce swelling.
- Anticoagulants: To prevent blood clots, a common complication due to protein loss.
- Infection Prevention and Treatment: Children with CNS are highly susceptible to infections due to protein loss and immune system issues.
- Nutritional Support: Ensuring adequate nutrition is paramount, as protein loss can lead to growth failure. This often requires specialized diets and sometimes tube feeding.
- Immunosuppressive Therapy (Limited Role): Unlike some other forms of nephrotic syndrome, CNS is generally not responsive to standard immunosuppressive medications (like steroids) because it’s typically caused by a structural genetic defect rather than an immune attack. However, in very specific genetic subtypes or if a secondary immune component is suspected, they might be tried.
- Bilateral Nephrectomy (Kidney Removal): For children who don’t respond to other therapies and continue to have severe protein loss and complications, surgical removal of both kidneys may be considered. This eliminates the source of protein loss and makes fluid management easier, preparing the child for future kidney replacement therapy.
- Kidney Replacement Therapy: This is the long-term definitive treatment for most children with CNS, as their kidneys eventually fail.
- Dialysis: Peritoneal dialysis (PD) is often preferred for infants and young children, providing ongoing blood filtration at home. Hemodialysis is another option.
- Kidney Transplantation: This is the ultimate goal, offering the best long-term quality of life. The timing of transplantation depends on the child’s overall health and growth.
NephCure Inc. plays a vital role in supporting research into the genetic basis of conditions like CNS, improving early diagnosis, and fostering better long-term outcomes through patient support and advocacy for innovative Congenital Nephrotic Syndrome treatment strategies.
Driving Towards a Cure: NephCure Inc.
The journey for patients with rare kidney diseases and their families can be incredibly challenging. At NephCure Inc., we are committed to transforming that journey into one of hope and progress. Our work spans funding cutting-edge research, advocating for new treatments, and building a supportive global community.
Here’s why patients, families, and researchers trust NephCure Inc.:
- Unwavering Focus: We are singularly dedicated to finding treatments and cures for rare, protein-spilling kidney diseases.
- Funding Breakthrough Research: We strategically invest in the most promising scientific investigations that explore disease causes and potential therapies.
- Patient-Centric Advocacy: We amplify the patient voice, advocating for faster drug development, equitable access to care, and supportive policies.
- Global Community Building: We connect patients, families, clinicians, and researchers, fostering collaboration and shared knowledge.
- Driving Innovation: Our work directly contributes to advancements in understanding and treating complex conditions.
Don’t let the complexity of kidney disease overshadow the hope for better treatments and cures. Every step in research brings us closer to a future where these conditions are manageable or even curable.
Ready to learn more about our mission or get involved? Contact NephCure Inc. today! Whether you’re interested in the latest on Focal Segmental Glomerulosclerosis causes, breakthroughs in C1q treatment, or advancements in Congenital Nephrotic Syndrome treatment, we’re here to share knowledge and build a healthier future, together!




